New guideline reduces repeat lumpectomies
A new guideline for determining whether enough tissue has been removed during breast cancer lumpectomy procedures significantly reduces the number of reoperations and lowers costs, according to a study by Washington University breast cancer surgeons.*
In a lumpectomy, surgeons remove the tumor plus a margin of surrounding healthy tissue. Pathologists cover the outside of the excised lump in ink, slice it, and examine the slices under a microscope to determine the size of the margin. If the margin is too small, the patient undergoes a second operation to remove more tissue.
Until recently, there has been disagreement about how wide that margin needed to be. Then in 2014, the Society of Surgical Oncology (SSO) and American Society of Radiation Oncology (ASTRO) issued a consensus guideline known as the “no ink on tumor” standard. Under this guideline, if there is no ink on the tumor, a second operation is unnecessary; wider margins do not lower the risk of recurrence.
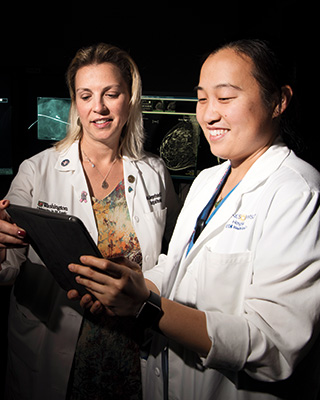
“We adopted the standard quickly,” says breast surgeon Julie Margenthaler, MD. “In addition to the potential for cost savings, it represents a big improvement in quality of care. Second surgeries cause anxiety, lost time from work and delays in starting chemotherapy and radiation.”
To measure cost savings, Margenthaler and general surgery resident Jennifer Yu, MD, MPHS, reviewed 1,506 cases conducted between 2010 and 2013, pre-guideline, at Barnes-Jewish Hospital. They found that, had the new guideline been in place, it would have avoided 87 reoperations at a total cost of roughly $195,000 — reducing the rate of reoperations by 5.6 percent.
“We will never get the reoperative rate down to zero, because we don’t have anything in the operating room to measure margins,” says Margenthaler. “Despite everything you do, some tumors will still have positive margins. But under the new guideline, we have reduced our rate of reoperation from about 20 to 30 percent to about 10 percent, which provides a significant reduction in cost and anxiety over past practices.”
*Yu J, Elmore LC, Cyr AE, Aft RL, Gillanders WE, Margenthaler JA. Cost Analysis of a Surgical Consensus Guideline in Breast-Conserving Surgery. J Am Coll Surg. 2017 Aug;225(2):294–301
Highlights

REBECCA AFT, MD, PHD, and colleagues reported on using a microfiltration technique to analyze disseminated tumor cells (DTCs) in the bone marrow of breast cancer patients, where their presence indicates a high risk of cancer recurrence. The microfiltration technique provided a more sensitive and accurate way to detect DTCs in bone marrow, an ability that should improve detection of early recurrence. The technique also identified two genes that are potential therapeutic targets. PLOS ONE published the study in January 2017.
A PERSONALIZED VACCINE for pancreas cancer, developed by William Gillanders, MD, and Robert Schreiber, PhD, professor in the Department of Pathology and Immunology, will be the focus of a clinical trial approved by the National Institutes of Health (NIH). The researchers developed the vaccine under a Pancreatic Cancer Specialized Programs of Research Excellence (SPORE) grant at Washington University.
PHOTOACOUSTIC IMAGING uses light and sound to produce images useful in distinguishing cancer from normal tissue. The technology may enable surgeons to gauge the success of lumpectomies while the operation is still underway, rather than relying on pathology results that come in after the fact. Former Washington University biomedical engineer Lihong Wang, PhD, now at Caltech, developed the technology and is investigating its use in the operating room; Aft recently coauthored a paper in Science Advances reporting that photoacoustic imaging provides images similar in quality to the histological images currently used to determine whether all cancer has been removed — an early proof-of-concept of the technology’s clinical value.
 In memory:
In memory:
Jeffrey F. Moley
Jeffrey Fletcher Moley, MD, chief of the Section of Endocrine and Oncologic Surgery, died Sunday, Oct. 15, 2017, at his home in Kirkwood, Missouri. He was 64.